Unveiling the Role of the MoCA Test in Identifying Progressive Supranuclear Palsy
Progressive Supranuclear Palsy
PSP is a less common form of neurodegenerative disease, which affects the functioning of the brain by causing nerve cell deterioration. It is categorized under 'parkinsonism', which refers to conditions that exhibit Parkinson's-like symptoms but are more resistant to conventional Parkinson's disease treatments.
The initial symptoms of PSP often involve loss of balance, frequent falls, and difficulty controlling eye movement. As the disease progresses, individuals may face challenges with swallowing, speaking, and cognitive skills, making it increasingly difficult to perform daily activities.
The MoCA Test
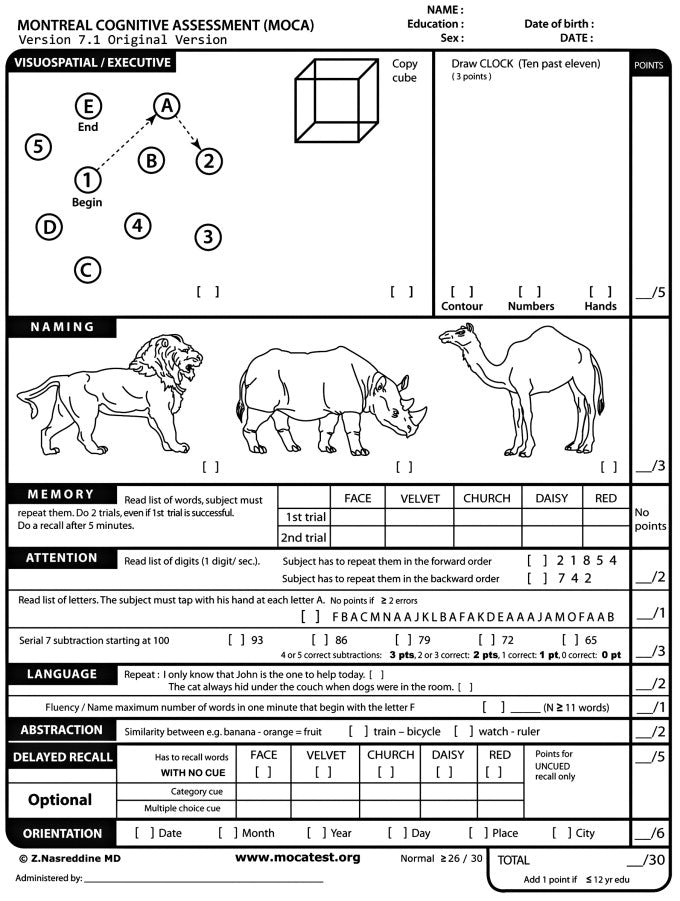
The Montreal Cognitive Assessment, or MoCA, is a cognitive screening instrument designed to assist health professionals in detecting cognitive impairment. It evaluates different types of cognitive abilities, including memory, executive functions, visuospatial abilities, language, and orientation to time and space. Its sensitivity in identifying mild cognitive impairment has proven to be significantly higher than other tools, making it a popular choice in clinical and research settings.
MoCA and PSP
The role of MoCA in identifying PSP is twofold. Firstly, it helps to reveal cognitive changes, which are often a part of PSP, albeit less recognized than motor symptoms. PSP patients may exhibit cognitive impairment, including slowed thinking (bradyphrenia), difficulty multitasking, or language problems. By assessing various cognitive domains, the MoCA test can help pinpoint these issues.
Secondly, while there isn't a specific cure for PSP, early detection can lead to better management of the condition. Recognizing cognitive impairment may aid in the early diagnosis of PSP when other symptoms such as falls or problems with eye movements are present.
The use of the MoCA test in PSP patients has been backed by scientific studies, demonstrating its utility in identifying cognitive impairment in this group. However, it's important to remember that MoCA is a screening tool, not a diagnostic one. A comprehensive clinical evaluation, alongside other diagnostic tests, is crucial in diagnosing PSP or any other neurodegenerative disease.
The cognitive impairment in PSP tends to be somewhat unique in its pattern, often involving executive functions and slowing of thought processes, rather than memory impairment typically seen in conditions like Alzheimer's disease. This makes the MoCA test, with its focus on multiple cognitive areas, a helpful instrument in identifying and characterizing the cognitive aspects of PSP.
The MoCA test has brought significant strides in the early detection and management of various cognitive impairments, including those caused by PSP. As our understanding of PSP and its effects on cognition continue to evolve, tools like MoCA will only become more valuable. Nonetheless, further research is necessary to perfect our approach to diagnosing PSP, ensuring patients receive the right support and management as early as possible.

 Donate
Donate